by Merrill Goozner
GoozNews
Hospitals are pushing again on an experiment that might put suppliers on budgets. CMS ought to ignore their lobbyists and consultants taking part in video games with numbers.
Altering the best way hospitals and docs receives a commission is central to reforming our dysfunctional well being care system. Fee reform can obtain higher well being outcomes, enhance the affected person expertise and assist hold general well being care prices in examine, the three targets of any reform worthy of the identify.
I’m a partisan on this debate. Practically two years in the past, I co-wrote a two-part collection in Well being Affairs (right here’s Half 1 and Half 2) touting Maryland’s fee system, which options widespread costs for all payers and capped hospital budgets. The four-person group was led by Dr. Ezekiel Emanuel of the College of Pennsylvania, a frequent advisor to Democratic administrations on well being care coverage.
Underneath all-payer pricing, hospitals cost each payer — whether or not a non-public insurer, Medicare, Medicaid, the Veterans Administration, or individuals with out insurance coverage — the identical worth for a similar service. In each different state, hospitals cost various charges: The uninsured pay the very best costs; personal insurers (or, to be extra exact, the employers and particular person prospects who purchase their insurance policies) pay on common 2 1/2 instances what Medicare pays; and Medicaid and the VA pay the least.
Because the late Seventies, Maryland has retained a state-appointed fee (The horror! Authorities regulation!) to set hospital charges. Particular person hospitals come earlier than the Well being Providers Price Evaluate Fee when they need a charge improve, identical to some other public utility. The hospitals doc their prices and the fee units charges that allow the establishment to pay its payments and earn a small revenue (or pad the endowment-like wet day funds of non-profit hospitals, which most are).
Through the previous decade, Maryland made two main revisions to its all-payer pricing mannequin, largely as a result of hospitals had prevented its rate-control virtues by growing the amount of providers they delivered. In 2014, the state set funds caps for its hospitals, which restricted their income development annually to a share set by the fee. And in 2018, the state, with the federal authorities’s blessing, took their mannequin one step farther: It set limits on the complete price of care (not only for hospitals however all medical providers) for its Medicare beneficiaries.
Underneath this newest permutation of Maryland’s program, hospitals that maintain complete Medicare prices in examine share these financial savings with the doctor practices, nursing properties and different suppliers that collaborate in holding these prices beneath a set funds. This system additionally elevated funding in main care practices, giving these comparatively low-paid physicians the monetary assist wanted to coordinate care for people with complicated medical wants.
In conducting a evaluation of the Maryland expertise, I spent weeks pouring over opinions performed by exterior evaluators employed by the Facilities for Medicare and Medicaid Providers. CMS’ beancounters wished to know whether or not authorities’s paying for the precise price of care (establishing the identical costs for presidency and personal payers), when coupled with international budgets, had really succeeded in limiting the expansion in general spending for Medicare beneficiaries. (As a result of all-payer pricing ends cost-shifting between varied payers, the federal government pays Maryland hospitals extra for Medicare and Medicaid beneficiaries than it does in different states. The flip aspect is that the privately insured pay much less.)
The reviewers answered within the affirmative. “Between January 2014 and June 2018, uniform ‘all-payer’ pricing inside hospitals coupled with international hospital budgets lowered Medicare spending in Maryland by almost $1 billion, or about 10% of complete hospital spending within the state, the evaluation concluded. Additionally they discovered that industrial insurers paid charges per inpatient admission that had been 11 % to fifteen % decrease than what these insurers paid comparable hospitals in different states. (Extra on utilizing comparable hospitals to measure success or failure fairly than per capita spending in a second.) These decrease costs had been offset by the upper costs Medicare and Medicaid paid.
Given these outcomes, CMS, which underneath the Inexpensive Care Act was empowered to experiment with varied fee reforms, known as Maryland’s all-payer pricing/funds cap system its most profitable different fee experiment.
Final October, CMS’ Innovation Middle adopted up by unveiling an experimental program that may enable as much as eight different states to undertake variations of the Maryland mannequin. Dubbed AHEAD (for All-Payer Well being Fairness Approaches and Improvement), the company will announce its first planning grant winners in July, a spokeswoman for the company advised me this week.
Business pushback
As I famous in my story final October after the brand new program was introduced, CMS didn’t embody essentially the most radical side of Maryland’s regulatory regime — all-payer worth setting. That will require an act of Congress since setting a single worth for every service would require elevating Medicare and Medicaid charges to offset the autumn in industrial charges, one thing that even a Democratic Occasion-led Home and Senate would discover troublesome to embrace given the ability of the hospital and insurance coverage lobbies in Washington.
That’s unlucky. The financial savings from all-payer pricing could be huge. It will sharply cut back bloated administrative prices since hospitals would not have to keep up a dozen or extra worth schedules. It will put an finish to the kabuki drama of insurer-hospital worth negotiations that routinely comes up with worth will increase greater than underlying inflation.
However all-payer pricing was the bridge too far for the CMS Innovation Middle. It will require growing authorities spending to gross up Medicare and Medicaid. It will require capturing employer financial savings by means of greater taxes on income and wages (employers might keep away from greater taxes by including their medical health insurance financial savings to staff’ paychecks, which is the place they rightfully belong).
The Biden administration’s try to advertise a extra reasonable model of the Maryland mannequin didn’t assuage the hospital {industry}. Chip Kahn, CEO of the Federation of American Hospitals, which represents for-profit hospitals, instantly attacked the brand new program. “Global budgets, the foundation of the model, are the wrong way to go and are more likely to cause issues with access to care and stifle innovation as they are to hold down costs and improve quality and equity,” he stated. “The evidence on this type of experiment is less than compelling.”
Then, final month, an article attacking this system by {industry} marketing consultant Jeffrey Goldsmith appeared on the web site of the Healthcare Monetary Administration Affiliation, which represents hospital finance officers. This week, Goldsmith, whose analysis was funded FAH, adopted up with an article on his personal web site.
He relied on information posted on the Kaiser Household Basis web site that studies the common price of care for people (per capita spending) in each state within the union going again to 1991. Goldsmith in contrast Maryland’s development in per capita spending over the following 30 years to the nationwide common and to 5 different states (neighboring Pennsylvania and Virginia, and Wisconsin, Minnesota and Oregon, which have a big share of their populations underneath insurance coverage industry-led managed care).
“Despite Maryland’s long history of regulatory oversight of hospital rates, healthcare costs in the state in 2020 were higher, not lower, than the national average, and they have grown at virtually the same rate as the overall national rate over the past 30 years,” he stated.
He additionally analyzed the expansion in personal well being care spending by taking a look at per capita prices for people who find themselves privately-insured, that’s, not coated by Medicare, Medicaid or different government-funded packages. That KFF information on personal spending solely goes again to 2001. Once more, he discovered that Maryland’s system, although “designed to minimize cost shifting to employers” has per capita personal insurance coverage well being prices “higher than the national average and have grown at a faster rate than in the country as a whole.”
Enjoyable with numbers
So much can occur in 20 or 30 years, and quite a bit did occur to Maryland’s program since 1991. However to know the evolution of this system, it’s important to return to its beginnings within the Seventies to know why Goldsmith’s numbers, whereas superficially correct, are deceptive.
Right here’s the temporary define. The onset of charge regulation and all-payer pricing in 1974 had its supposed impact virtually instantly. Maryland’s per capita spending on well being care went from ninth highest amongst all states and a pair of.4% above the nationwide common in 1972 to 14th ranked and simply 1% above the nationwide common a decade later, in response to older CMS information revealed in 1985.
However over the following three many years, two issues occurred that undermined charge regulation. First, the hospital {industry} embraced the deregulatory fervor of the Reagan period. Its leaders lobbied state legislators to finish worth oversight within the 27 states the place it had been adopted. Maryland’s regulators, one among solely two states to keep up the regime, hesitated denying their hospitals the identical charge will increase that had been being “negotiated” between hospitals and insurers in neighboring states. Company seize was alive and nicely in Annapolis.
The second and extra vital issue was the rise of personal ambulatory surgical facilities, usually physician-owned. This moved a rising share of routine however profitable surgical procedures like colonoscopies, cataract removing, and orthopedic tendon restore exterior the 4 partitions of the hospitals and thus not topic to charge regulation. Maryland noticed extra development in ASCs than some other state within the nation.
By 2012, the 12 months earlier than the Inexpensive Care Act’s insurance coverage enlargement went into impact, per capita spending in Maryland had soared to eight.5% greater than the nationwide common. Nonetheless, the rise of ambulatory surgical facilities and its impression on rising well being care prices was taking place in each high-income state. Maryland really improved its state rating on per capita prices, falling one place to fifteenth amongst all states.
Nonetheless, the federal authorities, alarmed by the rise within the further funds for Maryland’s Medicare and Medicaid beneficiaries wanted to maintain hospital charges stage, threatened to finish the experiment. That’s when Maryland turned first to capped budgets for its hospitals and, since 2018, to its complete price of care mannequin, which includes suppliers exterior the 4 partitions of the hospital. By 2020, Maryland per capita spending ratio had fallen to six.4% above the nationwide charge and it lowered its rating amongst all states to sixteenth.
And it will be quite a bit nearer to the nationwide per capita spending charge if 11 states, principally from the outdated Confederacy, had expanded Medicaid and extra aggressively pushed individuals to join Obamacare plans on the federal or state exchanges. Having medical health insurance will increase per capita spending on well being care. The truth that a few of the largest and wealthiest states within the nation (Texas, Georgia and Florida, particularly) are also among the many states with the very best uninsured charges reduces per capita spending in these states and drags down the nationwide common.
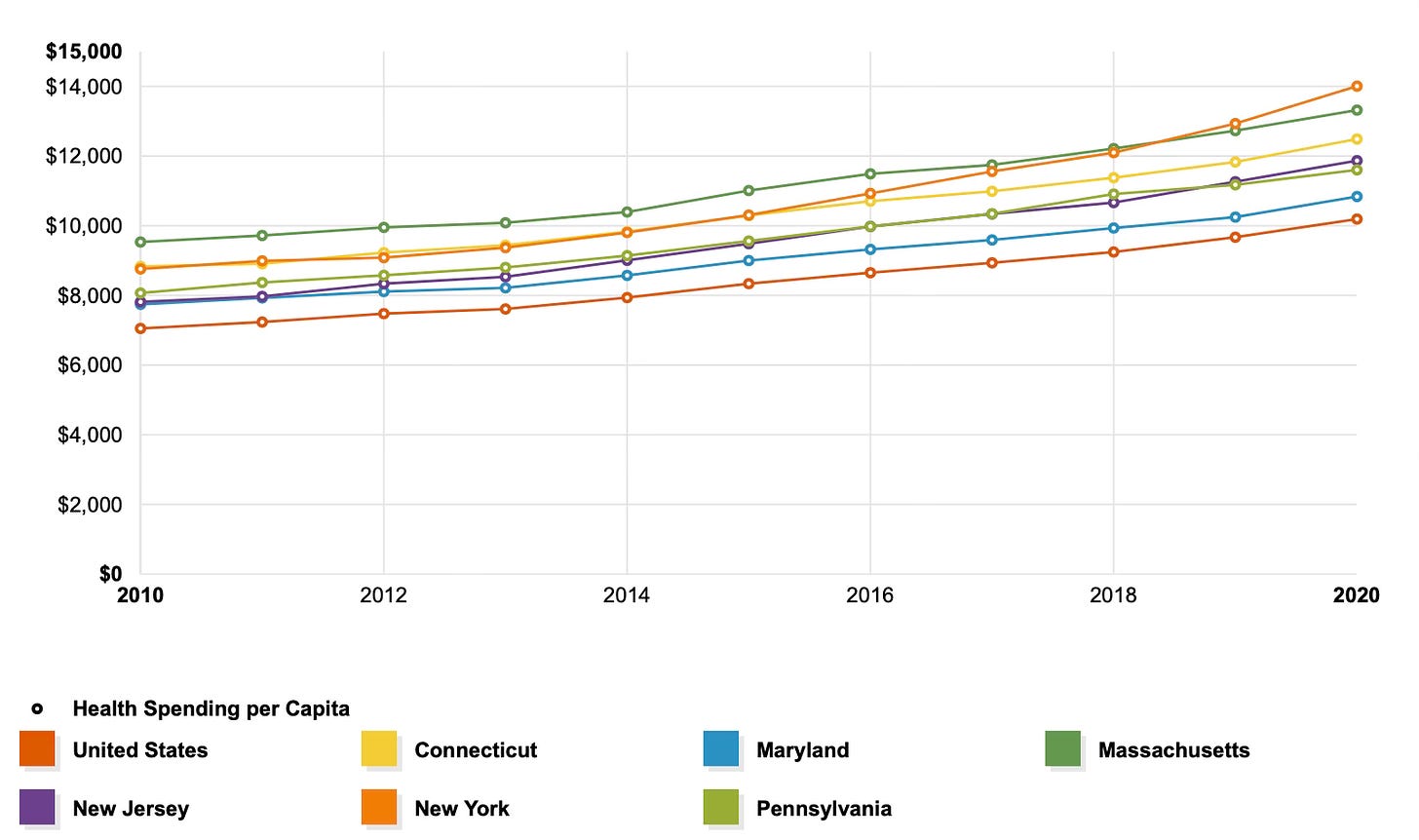
A great way to see the impact of Maryland’s expertise within the final decade (when it coupled capped budgets for hospitals with all-payer worth setting) is to check the expertise of Maryland and 5 different states — like Goldsmith — however to not its instant neighbors or states with a heavy presence of managed care. Let’s have a look at states which can be like Maryland in earnings and training; are geographically a part of the identical area; have plenty of high-cost educational medical facilities; and have a number of excessive poverty city cores. I selected Massachusetts, Connecticut, New York, New Jersey and Pennsylvania (additionally in Goldsmith’s pattern).
The next chart, produced by the KFF web site, covers the primary decade after the Inexpensive Care Act handed:
Each state within the Northeast and mid-Atlantic area started the last decade with per capita well being care prices above the nationwide common (the purple line on the backside). Maryland (the blue line) in 2010 was about equal to New Jersey and Pennsylvania. However beginning in 2012 and yearly thereafter, Maryland’s prices rose at a slower charge than its regional friends. And should you look intently, Maryland international budgeting/complete price of care experiment really narrowed the hole between the state’s per capita spending and the nationwide common.
All payers should be concerned
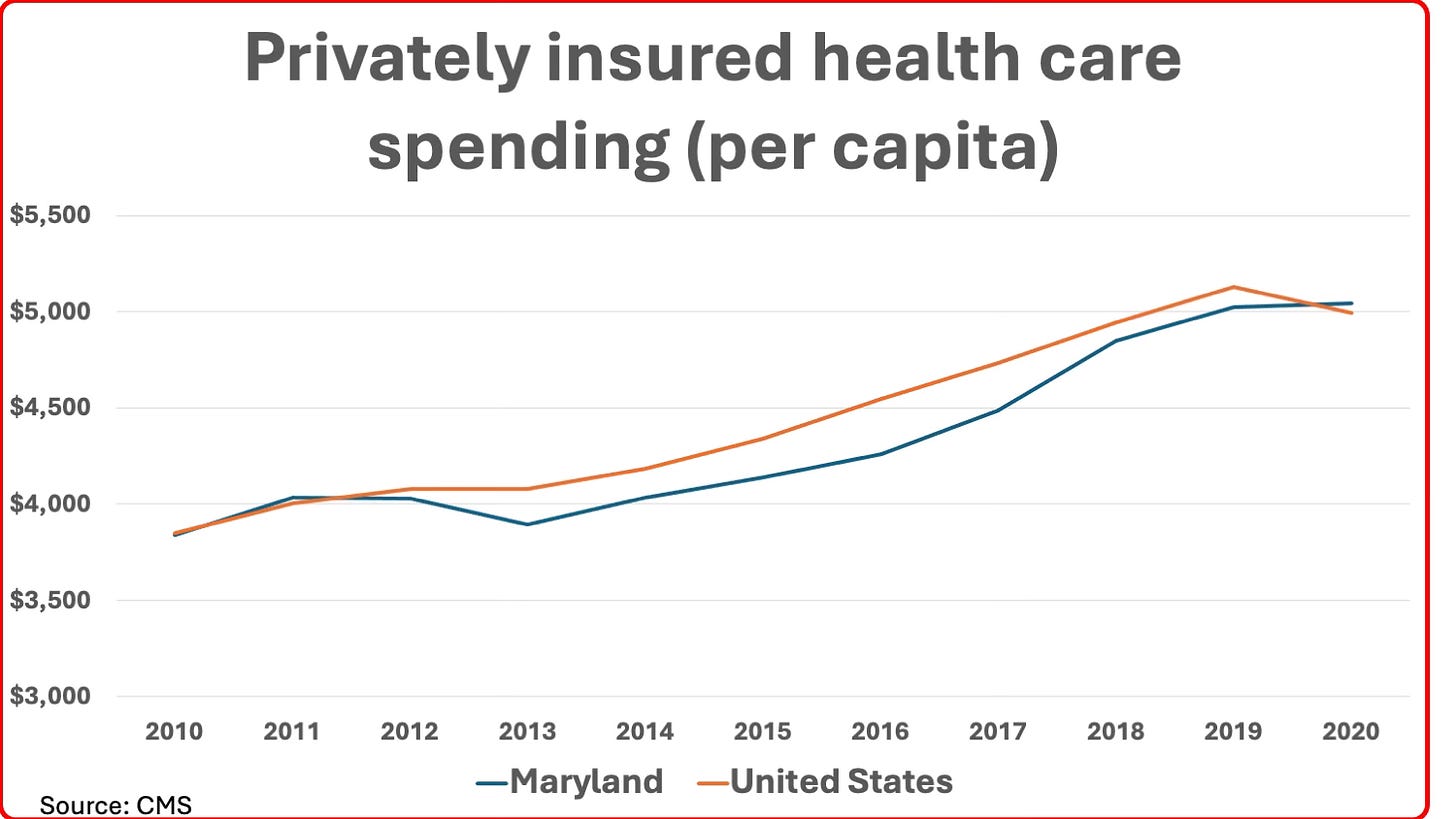
How about Goldsmith’s different main level: That Maryland’s personal insurers (and their employer and particular person prospects) incurred greater prices per capita over the previous twenty years than both its neighboring states (Pennsylvania and Virginia) or the nationwide common? An in depth have a look at the numbers exhibits this was, actually, a really latest phenomenon and simply explainable.
If I had drawn the above chart utilizing information from 2001 (the primary 12 months privately-insured per capita spending is offered from CMS), it will have proven that on the daybreak of the brand new millennium, Maryland’s per capita prices for the privately-insured was 5.6% beneath the nationwide common. This start line — not talked about in Goldsmith’s article — is testimony to the preliminary energy of all-payer pricing to scale back charges for the privately insured. As I famous earlier, Maryland had among the many nation’s highest charges for the privately insured previous to the daybreak of its regulatory system within the Seventies.
This held for many of the subsequent decade, though the unfold narrowed considerably through the steep recession of 2008-2010 and had virtually disappeared by the point the ACA handed in 2010 due to the rise of ASCs. When Maryland adopted capped budgets for hospitals starting in 2013, the charges for personal insurance coverage as soon as once more fell beneath the nationwide common — a reality documented by CMS’ reviewers by evaluating prices to comparable hospitals in different states. It was solely within the final two years of the final decade that Maryland’s per capita prices for the privately insured started rising once more and reached, in 2020, the marginally greater price in comparison with the nationwide common famous by Goldsmith.
Why did that occur? Easy. In 2018, Maryland and CMS agreed to its complete price of care mannequin. However it solely utilized to Medicare’s fee-for-service beneficiaries — not the privately insured or Medicare Benefit sufferers, whose ranks had been rising quickly. Hospital techniques and different suppliers little question focused on holding down the full price of take care of this narrower group by means of higher care coordination and eliminating pointless hospitalizations. With FFS Medicare utilization in decline, the Maryland fee raised charges for all payers to make sure hospitals obtained their annual budgets.
Certainly, this adjustment accelerated through the pandemic, when discretionary use of hospital providers collapsed and hospitals throughout the nation — not simply in Maryland — confronted a monetary disaster that required an enormous bailout from the federal authorities. As I famous in a GoozNews article in February 2021 reporting on a analysis letter that appeared in JAMA, Maryland had the regulatory construction in place to lift charges for all its payers to assist make up the shortfall.
Goldsmith concluded his article by claiming “the era of hyperinflation in health costs is over.” The true crises, he writes, “are affordability, declining life expectancy and huge gaps in care for the mentally ill and those requiring primary care.”
I’ve no quarrel with these priorities. Plus I assist his prescription for limiting out-of-pocket bills for all sufferers to a low share of complete earnings irrespective of how excessive the invoice. However he’s untimely in declaring an finish to the period of hospital and different suppliers’ worth hikes and quantity inflation.
The newest financial indicators report from the non-profit Altarum confirmed the patron worth index for hospital and associated providers soared 7.9% up to now 12 months. The CPI for well being care general (hospitals, doctor workplaces, labs, nursing properties, and many others.) was up simply 2.8%, however when coupled with hovering volumes (up 4.3%) mixed to ship general well being care prices up 6.7% — greater than inflation plus financial development.
International budgeting that impacts each side of well being care supply has the best potential to restrict hospital utilization, which stays the one largest expense in well being care.
It some methods, it will be like Medicare Benefit, the place personal insurers obtain a set funds for all Medicare beneficiaries of their plans after which restrict spending utilizing instruments like prior authorization, step remedy and outright denials of care. I’d fairly give supplier organizations the fastened funds and let their medical professionals make these choices.
I conclude by noting essentially the most salutary impact of fastened budgets. They might promote higher well being by giving supplier organizations the ability to allocate sources. They may spend extra on prevention, main care, behavioral well being and the social providers that may hold individuals out of the hospital.
However to ensure that that to succeed, the worldwide funds/complete price of care mannequin should cowl each payer, not simply Medicare beneficiaries as in Maryland. CMS made a clever selection when it insisted in its name for AHEAD functions that at the least one insurer be included in each proposal.