On revenue uncertainty and ACA market software (substack.com) xpostfactoid Andrew Sprung
Brian Blase, a conservative healthcare scholar on the Paragon Institute, is out with an evaluation of 2024 ACA market enrollment (summarized on this WSJ op-ed) claiming that tens of millions of enrollees have mis-estimated their incomes to say advantages to which they’re “not entitled.” Listed below are the core claims:
In 9 states (Alabama, Florida, Georgia, Mississippi, North Carolina, South Carolina, Tennessee, Texas, and Utah), the variety of sign-ups reporting revenue between 100% and 150 % FPL exceed the variety of potential enrollees. The issue is especially acute in Florida, the place we estimate there are 4 occasions as many enrollees reporting revenue in that vary as meet authorized necessities.
The issue of fraudulent alternate enrollment is rather more extreme in states that haven’t adopted the ACA’s Medicaid enlargement in addition to in states that use the federal alternate (HealthCare.gov). In states that use HealthCare.gov, 8.7 million sign-ups reported enrollment between 100% and 150 % FPL in comparison with solely 5.1 million folks doubtless eligible for such protection, or 1.7 sign-ups for each eligible particular person….
Unscrupulous brokers are actually contributing to fraudulent enrollment and the improved direct enrollment function of HealthCare.gov seems to be an issue. Brokers simply want an individual’s title, date of beginning, and deal with to enroll them in protection, and studies point out that many individuals have been lately faraway from their plan and enrolled in one other plan by brokers who earn commissions by doing so.
Blase’s core conclusions — that advantages beneficiant sufficient to induce the uninsured to entry them needs to be scaled again, and that efforts to streamline enrollment needs to be broadly rejected — are unwarranted, as argued beneath. His use of the time period “fraud” is overbroad. However he does level to weaknesses in enrollment safety and incentives to agent malfeasance which are mirrored in enrollment knowledge and have to be addressed.
First, the power of brokers to entry present accounts or create new ones with out verifiable enrollee consent, coupled with subsidy boosts enacted in March 2021 that rendered further tens of millions eligible without cost protection, has opened an avenue for fraud that’s been exploited in in all probability a whole lot of 1000’s (not tens of millions) of accounts within the 32 states utilizing the federal alternate, HealthCare.gov. CMS should shut down the fraud, and rapidly — working with brokers, state insurance coverage departments, insurers and business web-brokers — in addition to implementing a tech repair (I’ve written in regards to the agent/dealer scandal and proposed options right here, right here, right here, and right here.).
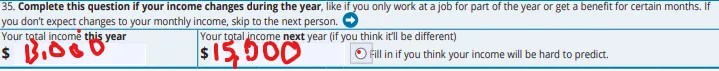
Second, brokers and to some extent nonprofit assisters probably do lead some enrollees to therapeutic massage their revenue estimates, and, as Blase avers, they’ve for the reason that market’s launch within the fall previous to Plan 12 months 2014. That’s inevitable in a system that 1) bases advantages on future revenue projections, 2) primarily serves low-income folks, whose revenue typically fluctuates and is tough to foretell, and three) contains revenue break factors the place advantages change considerably — together with, most radically, whether or not advantages can be found in any respect, i.e., the 100% FPL minimal revenue requirement in states which have refused to enact the ACA Medicaid enlargement. As extra brokers have piled into the market (there have been 83,000 registered with HealthCare.gov in 2024, up from 49,000 in 2018), projected revenue massaging might have elevated, although CMS knowledge breaking out enrollment by revenue doesn’t unequivocally help that conclusion (extra on that beneath).
Third, not less than one a part of one administrative rule designed to scale back enrollment friction and scale back the uninsured price, carried out after subsidies have been expanded in March 2021, has probably stimulated unauthorized (and fraudulent) plan-switching by brokers. In early 2022, CMS launched a steady Particular Enrollment Interval (SEP) — successfully year-round enrollment — for candidates with revenue beneath 150% FPL, who, due to the ARPA subsidy will increase, by that time had entry to a benchmark silver plan for zero premium. That’s within the spirit of year-round Medicaid enrollment, because the 150% FPL threshold isn’t a lot greater than the 138% FPL Medicaid eligibility threshold in nonexpansion states. The issue will not be with enabling the low-income uninsured to get protection year-round, however with permitting a month-to-month SEP that allows month-to-month plan-switching. That’s what rogue brokers have exploited.
That stated, Blase nearly actually exaggerates the extent of enrollment fraud and attracts largely incorrect conclusions from it. CMS ought to have the ability to get a deal with on unauthorized agent-executed plan-switching and enrollment. The 19 state-based marketplaces (SBMs) appear to have largely prevented it. Most likely at some price to enrollment progress. CMS might be making an attempt to strike a steadiness, adopting some requirement that an agent present proof of enrollee consent that generates much less friction than do SBM safety measures (e.g., requiring two-factor authorization from the shopper).
An outbreak of preventable agent fraud shouldn’t compromise or legislatively endanger extension of the improved premium subsidies quickly enacted within the American Rescue Plan’ Which such have introduced the Reasonably priced Care Act inside placing distance of dwelling as much as its title. These enhanced subsidies have been prolonged by means of 2025 by the Inflation Discount Act however will expire if not additional prolonged. Erasing zero-premium protection at low incomes would imply erasing protection beneficial properties which were a boon to tens of millions of low revenue enrollees.
It needs to be famous that a lot if not many of the impetus for agent fraud — plan-switching and enrollment not approved by the enrollee — would disappear if ten states weren’t stubbornly holding out towards the pursuits of their folks, their hospitals and their funds by refusing to enact the ACA Medicaid enlargement. In nonexpansion states, eligibility for market subsidies begins at 100% FPL, relatively than on the 138% FPL Medicaid eligibility threshold in impact in enlargement states.
Nonexpansion has created an enormous pool of enrollees who venture revenue within the 100-138% FPL vary. Individuals at or close to poverty belong in Medicaid, which is a less complicated, extra inexpensive (with near-zero out-of-pocket prices) and less expensive profit than market protection. If these states all enacted the enlargement tomorrow, greater than 6 million of the 9.4 million market enrollees who estimated revenue beneath 150% FPL (qualifying them without cost benchmark silver protection) would transition to Medicaid — radically shrinking {the marketplace} in these states and altering incentives for the massive name facilities which were concentrating on low-income market enrollees. However that speedy Medicaid enlargement will not be going to occur.