Middle for Healthcare High quality and Fee Reform CHQPR
I began reviewing rural hospitals a bit over a 12 months in the past. Not a lot has modified. These smaller hospitals lack for useful resource and manpower due to their funds restraints. Companies they supply is probably not coated by a affected person’s charges. In consequence, they’re at all times battling their funds. If they’re part of the 340B program and near a metropolis, bigger hospitals might purchase them out and take the good thing about the 340B. What stays is a shell of the previous hospital.
The next submit is a quick rundown of what’s want by these small hospitals. Extra later over the weeks.
Saving Rural Hospitals – Issues and Options for Rural Hospitals (chqpr.org)
A very good fee system for rural hospitals should obtain three key targets:
- Guarantee availability of important companies locally;
- Allow well timed supply of the companies sufferers want; and
- Help supply of applicable, prime quality, inexpensive care.
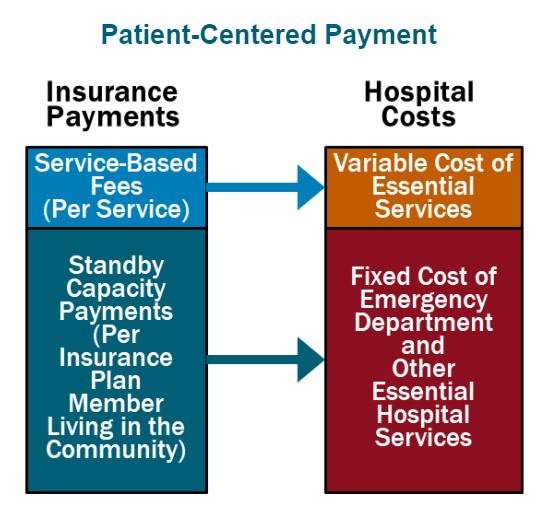
Affected person-Centered Fee for rural hospitals can obtain all three targets by means of the next 4 parts:
- Standby Capability Funds to Help the Fastened Prices of Important Companies. Every medical insurance plan (Medicare, Medicaid, Medicare Benefit, and business insurance coverage) ought to pay a Standby Capability Fee to the agricultural hospital primarily based on the variety of members of that plan who dwell locally (whatever the variety of companies the sufferers obtain). This ensures that the hospital has sufficient revenues to assist the minimal standby prices of important companies such because the emergency division, inpatient unit, and laboratory.
- Service-Primarily based Charges for Diagnostic and Remedy Companies Primarily based on Variable Prices. Rural hospitals ought to proceed to obtain funds from well being plans for delivering particular person companies, however beneath Affected person-Centered Fee, the Service-Primarily based Charges could possibly be a lot decrease than present funds. For the reason that hospital would obtain Standby Capability Funds to assist the mounted prices of important companies, the Service-Primarily based Charges would solely must cowl the extra prices incurred when further companies are delivered. Because of this if sufferers keep wholesome and wish fewer companies, the hospital’s revenues and prices will lower by related quantities, so the hospital’s margin won’t be harmed.
- Accountability for High quality and Spending. In return for receiving sufficient funds to assist important companies, rural hospitals ought to take accountability for delivering evidence-based companies safely and effectively.
- Worth-Primarily based Price-Sharing for Sufferers. TThe quantity {that a} affected person has to pay out of pocket to obtain vital companies ought to be inexpensive for the affected person, so sufferers will not be prevented from acquiring the care wanted to enhance their well being.
As well as, rural hospitals that function Rural Well being Clinics or major care practices should be paid for major care companies utilizing Affected person-Centered Major Care Fee. The clinic/observe ought to obtain month-to-month Wellness Care Funds and Power Situation Administration Funds to assist proactive preventive care and persistent illness care delivered by major care groups, relatively than being paid just for workplace visits with physicians/clinicians, in addition to Acute Care Go to Charges when sufferers expertise a brand new symptom or downside. The funds ought to present the clinic/observe with sufficient assets and adaptability to assist sufferers keep as wholesome as potential and to ship well timed, evidence-based care when the sufferers expertise well being issues.
This can be a patient-centered method to fee as a result of it’s designed to assist the companies that sufferers want, to not improve earnings for both hospitals or medical insurance plans. Affected person-Centered Fee would supply sufficient funding to assist companies in small rural communities with out the sorts of problematic incentives to ship pointless companies or to stint on care that exist in present fee programs and “value-based” funds.
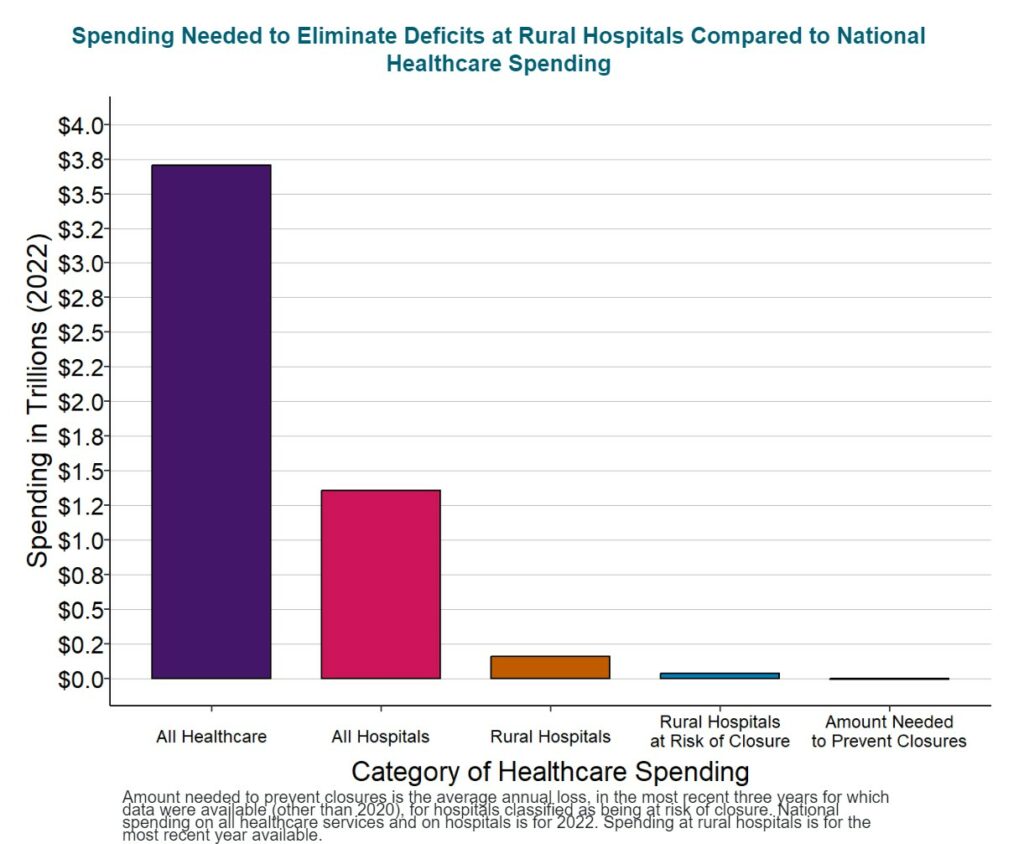
The way to Save Rural Hospitals and Strengthen Rural Healthcare
It would value about $4 billion per 12 months to forestall closures of the at-risk hospitals and protect entry to rural healthcare companies, an quantity equal to just one/10 of 1% of whole nationwide healthcare spending. No fee system will maintain rural hospitals and clinics until the quantities of fee are massive sufficient to cowl the price of delivering high-quality care in small rural communities. As a result of present funds are beneath the prices of delivering companies, a rise in spending by all payers shall be wanted to maintain rural hospitals solvent, however $4 billion is a tiny quantity compared to the greater than $3.3 trillion presently spent on healthcare and the greater than $1.3 trillion spent on all city and rural hospitals within the nation. Furthermore, many of the improve in spending will assist major care and emergency care, since these are the companies at small rural hospitals the place the most important shortfalls in present funds exist.
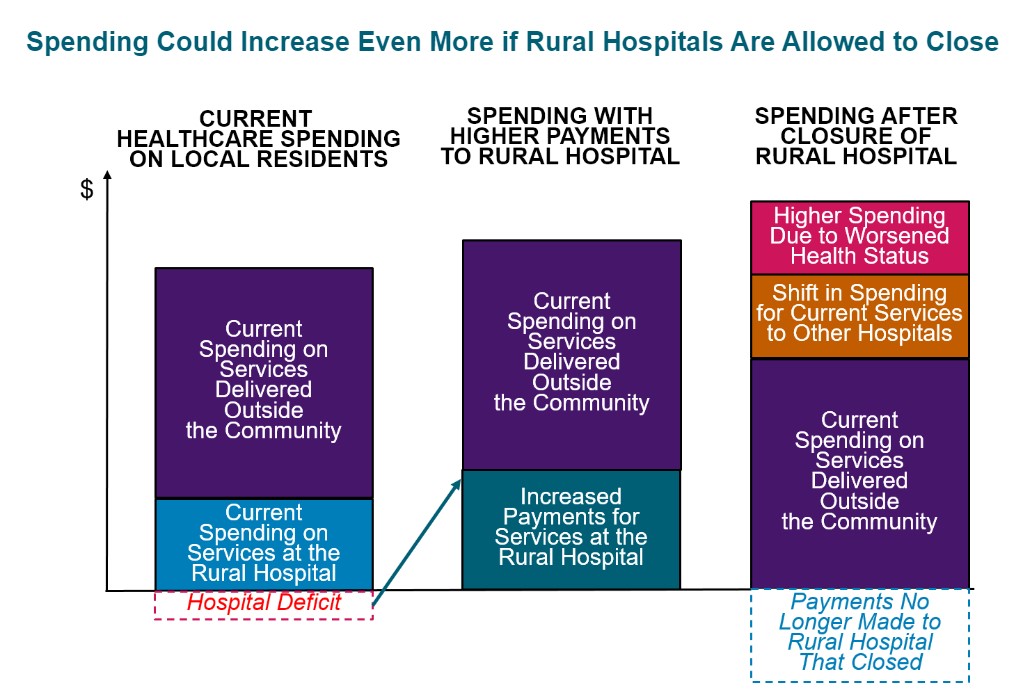
Spending would doubtless improve even when the hospitals shut. The diminished entry to preventive care and delays in therapy ensuing from a rural hospital closure will trigger residents of the neighborhood to want much more companies sooner or later. Paying extra now to protect native healthcare companies is a greater strategy to make investments assets.
Residents, companies, native governments, state authorities, and the federal authorities should all take motion to make sure that each payer gives sufficient and applicable funds for small rural hospitals and clinics:
- Companies, state and native governments, and rural residents should demand that non-public medical insurance firms change the way in which they pay small rural hospitals. The largest reason for adverse margins in most small rural hospitals in most states is low funds from personal insurance policy and Medicare Benefit plans. Non-public insurance coverage firms are unlikely to extend or change their funds until companies, state and native governments, and residents select well being plans primarily based on whether or not they pay the native hospital adequately and appropriately.
- State Medicaid packages and managed care organizations must pay small rural hospitals adequately and appropriately for his or her companies. Expanded eligibility for Medicaid will assist extra rural residents afford healthcare companies, however small rural hospitals can not ship the companies sufferers want if Medicaid funds are too low. CMS ought to authorize states to require Medicaid MCOs to make use of Affected person-Centered Funds and to pay adequately for companies at small rural hospitals.
- Congress ought to create a Affected person-Centered Fee program in Medicare for small rural hospitals. Though Medicare isn’t the first reason for deficits at small rural hospitals, Medicare must pay rural hospitals and clinics in a means that may higher maintain companies in the long term.
Rural hospitals should be clear about their prices, effectivity, and high quality, and they need to do what they will to manage healthcare spending for native residents.
With a purpose to assist increased and higher funds for hospitals, purchasers and sufferers in rural communities must believe the hospitals will use the funds to ship high-quality companies on the lowest potential value. That the hospitals will proactively determine and pursue alternatives to manage healthcare prices for neighborhood residents. Small rural hospitals ought to estimate the minimal possible prices for delivering important companies utilizing an goal methodology. They need to proactively work to enhance the effectivity of their companies, and they need to publicly report on the standard of their care.
- A “rural” hospital is a hospital positioned in an space that’s categorized as rural by the Well being Sources and Companies Administration. A “small” rural hospital is one which has whole annual bills beneath the median for all rural hospitals ($40 million in 2022).
Saving Rural Hospitals, The Disaster in Rural Well being Care (chqpr.org)